Boosting your Bottom Line Starts with Clean Claims
Charge scrubbing and claim submission is the most critical piece of information. Lost paper trails and lack of clarity of claim status results in delayed or lost revenue and disruptions in your cashflow. Electronic claim submission changes that by eliminating the manual paper-based claim processing and helps you get paid quicker.
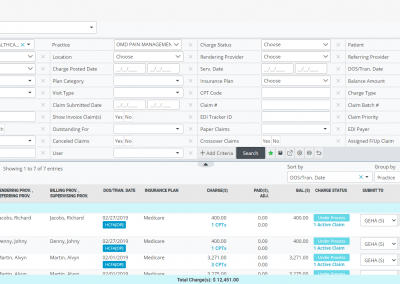
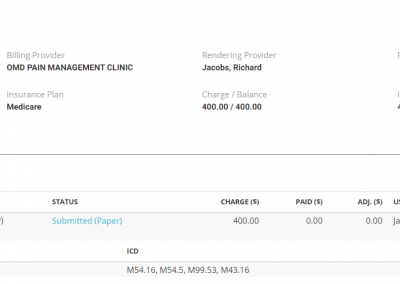
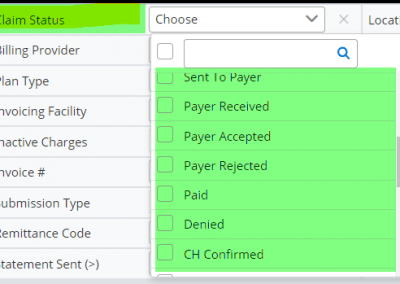
A greater than 5,000 commercial and government payers make it difficult for billers to keep track of every claim. OmniMD’s electronic claim manager follows a transparent digital status to each claim through status reports from the payer and clearinghouse.
The billers can still print paper claims when necessary and receive claim processing reports with status updates from clearinghouse and payer portals.
Submit Your Primary and Secondary Claims Directly.
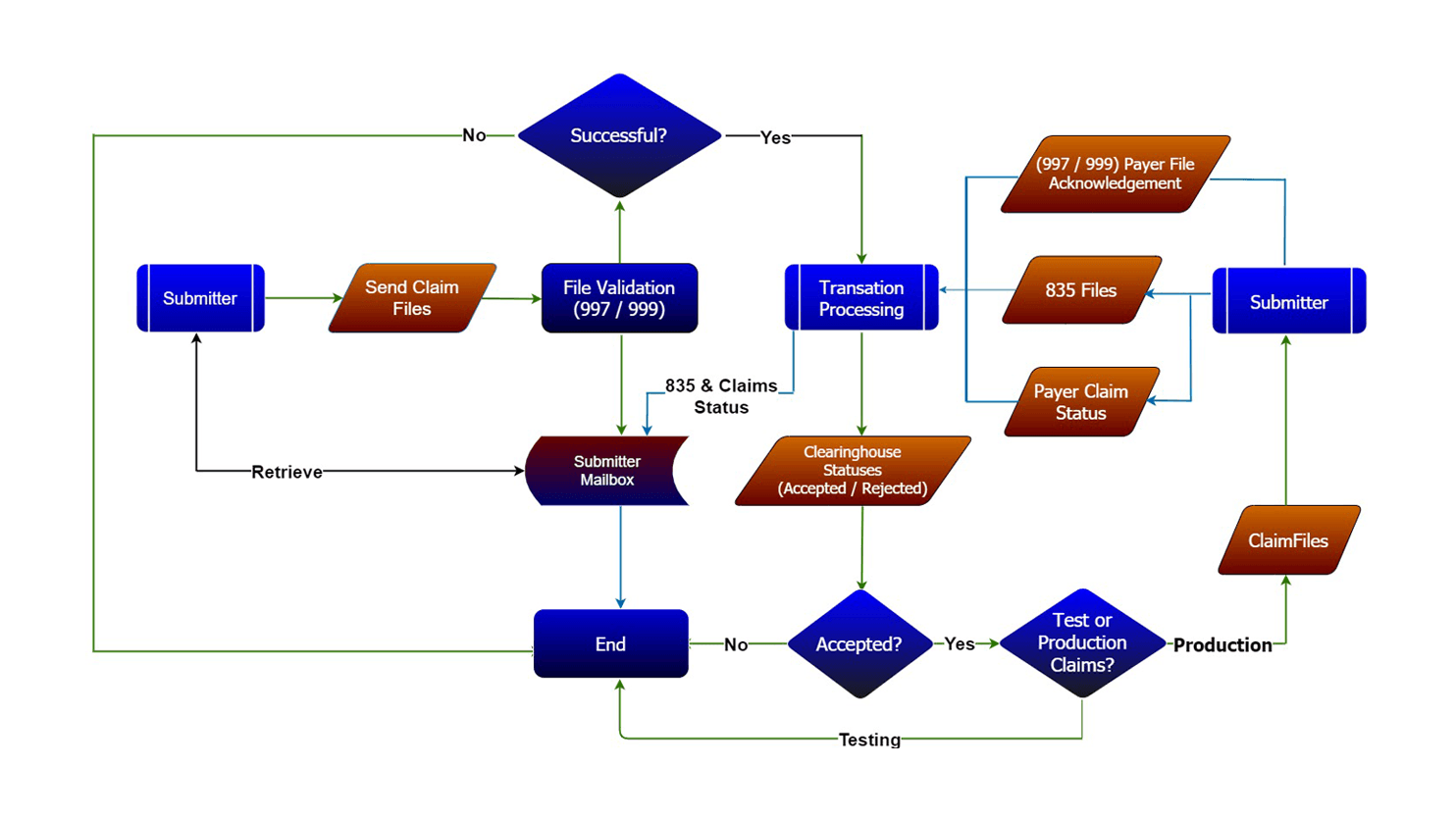
The Process
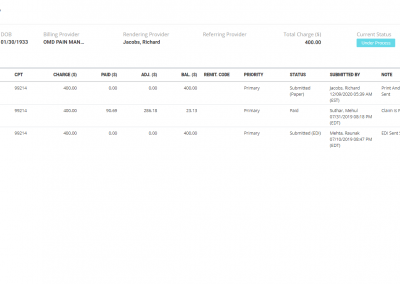
After entering changes, OmniMD RCM scrubs all claims against payer reimbursement rules (charge/claim scrubbing). Once the charges/claims are scrubbed, you can directly instantly submit primary, secondary, and tertiary electronic claims in the industry-standard ANSI 837P format from OmniMD to the government and commercial insurance companies nationwide without a direct connection with third-party medical clearinghouses. OmniMD provides the direct interface and access to these national clearinghouse services needed to submit claims electronically (learn more about your clearinghouse choices).
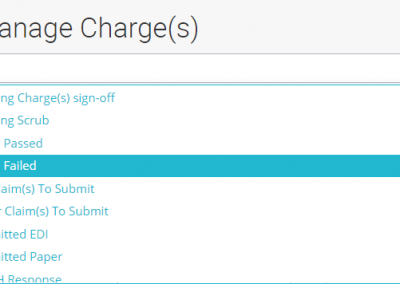
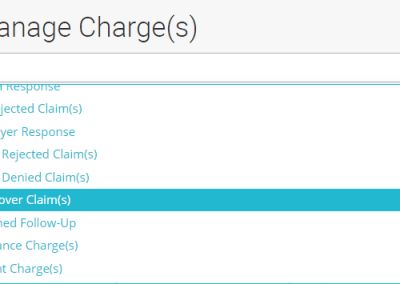
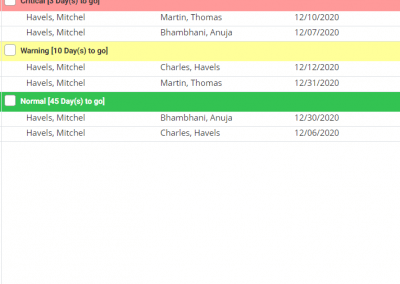
Charges/Claims rejected by clearinghouse
Charges/Claims without a payer response (based on a set number of days)
Charges/Claims rejected by the payer
Insurance Charges/Claims only
Patient Charges/Claims only
Crossover Charges/Claims
Claims pending to print
Claims already printed
Canceled Charges/Claims
Charges/Claims on hold
Cleaner the Claims, Higher the Reimbursements

OmniMD RCM adds to your peace of mind with multiple levels of reporting as your electronic claims pass through the claim submission and adjudication process. Each claim (paper and electronic) passes through a slew of scrubbing rules and yields validation reports to highlight claims with missing or invalid information, such as missing patient info, wrong payer ID, missing or wrong provider or group numbers, or incorrect policy numbers, etc. Once the claims pass through internal validation, your claims are forwarded to one of your preferred clearinghouses for further review (including CCI, HIPAA, LCD, and carrier-specific edits), which return daily reports that highlight claims that have been rejected for various payer-specific reasons. Once your claims get delivered to payers and get adjudicated, the payer responds with reports highlighting denied and paid claims. OmniMD RCM offers transparency from beginning to end for better efficiency, productivity, and greater peace of mind.





Tracking and Managing Rejections and Denials
OmniMD RCM tracks rejections and denials reported back through electronic claim processing and electronic remittance advice reports from insurance companies. Our system also offers comprehensive rejection and denial management reports to target specific rejections and denials in bulk efficiently. Claim and appeal filing alerts and notifications help your billing team address these denials and rejections in a timely fashion and avoid appeal timely filing limits.
In essence, with OmniMD RCM, you will save you considerable time, effort, and headache through our tracking and resubmission mechanism for rejected, denied, or no-response claims
What will you achieve with OmniMD RCM?
Electronic claim processing that minimizes disruptions to your cashflow and saves time and effort.
Track Claim status
Set timely filing limits for each payer
Build and track timely filing alerts and get notifications on login.
Build and appeal timely filing alerts and get notifications on login.
Multiple levels of claim status reporting
Individual and batch printing of paper insurance claims
Payer enrollment assistance
Up to 97% clean claim ratio
Build actionable worklists to manage rejections and denials
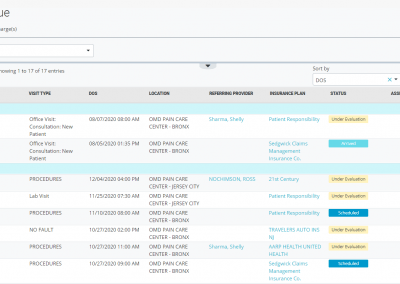
Worker’s Compensation and No Fault Claim Management
With OmniMD RCM and our association with Carisk, you can send worker’s compensation claim forms electronically along with medical records. You can customize and preset values in these forms for your provider and group within our intuitive settings.
Schedule a free demo and walk through the creation of solution from start to finish.
Learn More About Our Solutions
Send us an email or submit the form for more information.